In the first of this two-part series, we look at what we know—and don’t know—about concussions and brain injuries in equestrians.
At the U.S. Hunter Jumper Association Annual Meeting in December of 2016, a conference room overflowed with movers and shakers in the sport drained from days of committee meetings and impatient after being nagged into attending a presentation on concussions, of all things, as Lola Chambless, M.D., stepped on stage and turned on a slide.
“Of all the patients who are admitted to a hospital with a sports-related traumatic brain injury, how many do you think are equestrians?” she asked.
The New York Times had published more than 60 articles about football players and concussions in the last 11 months, and Time had recently equated the National Hockey League with big tobacco companies. Boxing experts were asking if the sport could even survive now that more information about the cumulative effects of repeated blows to the head was coming to light. Youth sports were similarly in near-crisis mode. But riding?
So in the wake of Chambless’ question the murmuring about dinner reservations didn’t dissipate—until she flipped the slide.
Forty-five percent, she said calmly. And that didn’t include all the concussions.
That did it: Chambless had everyone’s attention, in that room and, before long, far beyond it as attendees spread the word about equestrian head injuries. In later presentations Chambless would describe this as one of the most attentive and interactive audiences she’d ever worked with.
It didn’t hurt that Chambless wasn’t just another doctor. She was an eventer who grew up leaving her helmet in her tack trunk on occasion, ignoring physicians’ orders after injuries and picking up a few head injuries on her way to becoming a neurosurgeon at Vanderbilt University in Nashville, Tennessee. She’s also a mother whose child ended up in the hospital after a head injury. So when she wanted to talk about concussions and traumatic brain injuries in the horse world, and she began to challenge the deeply embedded ethos of “if you’re not calling an ambulance, get back on,” she had the necessary credibility to get horsemen to listen.
The Basics
The sport horse world has certainly suffered serious tragedies from head injuries and implemented helmet rules at shows to help prevent them. But new research about traumatic brain injuries, aka TBIs, and concussions, especially about their long-term effects, as well as changing thoughts on diagnosing and treating them, means concussion risks are now tack room chatter.
“Horsey people need to understand they have the highest rates of concussion, in any sport, anywhere in the world,” said Michael Turner, M.B.B.S., FFSEM, M.D., who was chief medical advisor to the British Horseracing Authority and currently serves as the medical director of the International Concussion And Head Injury Research Foundation. “Certainly race riding has the highest rates [one U.K. study puts the chance of a professional jump jockey falling in a race at one in 16, an amateur, one in eight], but even amateur equestrian sports have very high rates. We need to get out of the mindset that concussion is related to team sports.”
So what is a TBI?
Chambless described this as an umbrella term for a wide variety of brain injuries from mild concussions to severe coma, vegetative state or death. A concussion is a type of traumatic brain injury caused by a sudden movement (you don’t have to be hit on the head to experience a concussion) that causes the head and brain to move rapidly back and forth or twist
in the skull, creating chemical changes in the brain and sometimes stretching and damaging brain cells. Symptoms of a concussion include nausea, dizziness, headache, blurred vision and concentration or memory problems. Loss of consciousness only occurs about 9 percent of the time. Luckily it’s not hard to identify the symptoms. 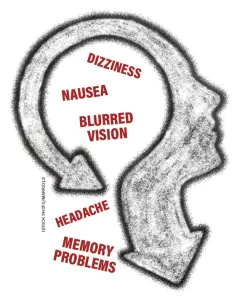
“A layperson’s assessment is going to be a conservative assessment,” said Chambless. “You’re going to tell people to be more worried than they need to be, but that’s where we want to go.”
Concussion symptoms may be slow to appear, and it’s recommended that anyone with a suspected concussion take at least a timeout.
“When I was young and stupid I would get right back on after I hit my head, and I realize that wasn’t the best thing for me or my horse,” said Chambless, of Nashville. “Nowadays I sit around and think about it for a few minutes, then proceed. I think changing the culture to allow for that would be helpful.”
The Latest On Head Injuries
Nowadays most concussion research focuses on two topics: return to play and the long-term effects of head injuries, especially repeated head injuries, believed to cause chronic traumatic encephalopathy, a serious degenerative brain disease. Jockeys, in particular, are believed to be at especially high risk for CTE. More and more studies are showing that the effect of concussions is cumulative, decreasing overall cognitive and memory function, and someone who’s suffered one is four to six times more likely to suffer another. So keeping track of head injuries throughout a lifetime is especially important.
“We want to know if your daughter’s just fallen off the pony again, should you sell the pony and tell her to take up another sport?” said Turner.
ADVERTISEMENT
When it comes to return to play, the answers aren’t clear. Most concussion symptoms resolve in a week, but some will last much longer. So when to go back to the barn?
The National Football League, National Hockey League, Major League Baseball and National Basketball Association all use baseline cognitive testing and post-concussion testing to determine when a player can return, using a provider called ImPACT, which determines cognitive function via a test taken on a computer. Eventing has adopted a rule that uses an ImPACT test to determine when concussed riders may compete again.
During the symptomatic period after a concussion, doctors used to recommend complete rest in a darkened room for seven to 10 days, but now they’re swapping that recommendation to active rest.
“You can’t completely rest your brain,” said Turner. “It’s always working.”
Active rest means that after symptoms fade, one should ease into increasing activity, going back to rest if the symptoms reappear. That may take a day. It may take much longer. But Chambless recommends waiting to ride during this time.
“If you’re a soccer player, it’s easy to do drills before a game [to ease into the sport],” she said. “But it’s hard for an equestrian to get back on a horse and go on a trail ride. It’s all pretty low-key until the horse spooks. Make sure you’re back to normal activity before getting on.”
Researchers are also looking for biomarkers that indicate concussion, meaning that a blood or saliva test could determine if a rider is concussed. But there are millions of biomarkers, and while there have been some studies showing promise, no one has found the right one yet. Drug companies in particular have been exploring this route with a vengeance, searching for good results from so-called “lollipop tests.” They’re hoping to be able to swab the inside of someone’s mouth right on the field, with the color of the swab demonstrating whether the individual has suffered a concussion. Unfortunately, the drug companies keep the progress of their research close to the vest until it’s ready for prime time, so no one is collaborating, and there’s no way to know how well the tests are going.
There are plenty of other projects in the works aimed at diagnosing concussions (many well funded by the likes of the U.S. Department of Defense and the NFL), like creating helmets with sensors that can detect concussions and portable electroencephalogram machines that physicians can use on the field to assess for concussions, but nothing’s ready to hit the market yet.
Researching Risk Within The Equestrian World
Part of the problem is there’s little actionable research that’s publicly available specific to horse sports.
The study that came up with the 45 percent compared medical data from hospitals across the country over a nine-year period. It’s a great start, but it doesn’t provide details that could help equestrians. What were the riders doing before they ended up in the hospital? Trail riding? Taking a lesson at a summer camp? Competing in a Fédération Equestre Internationale show? More to the point, were they wearing an approved helmet?
Many hospitals record this information, but not consistently, and it’s not recorded in the study.
The general consensus is that only about 25 percent of horsemen wear helmets when riding, despite the fact that helmets reduce TBIs by around 50 percent.
“What we can’t extrapolate is relative risk,” said Chambless. “We don’t know in a scientific way what types of accidents are more prone to causing concussion or TBI—not to mention barn accidents. Part of the problem is that most concussions and TBIs happen outside competition and not necessarily in a formalized practice with a trainer like [with] NCAA and pro sports. Most happen in a barely-witnessed way.
“Most of the people running trauma centers don’t know very much about equestrian sports, and they don’t really know the questions to ask,” she added. “We’ve looked at it in our own center in Nashville. We’re a very horsey town, and even having years and years and reams of data, it’s hard to find much we can move forward with. I think it’s going to have to come from our own data, and here are the variables that we care about.”
But there’s hope. Roy Burek, managing director of Charles Owen helmets, has been collecting data.
The company’s accident replacement program requires participants to fill out an extensive accident report form and return the helmet to the factory, which gives Burek more detailed information about falls. Having the form and the helmet—Charles Owen receives about three a day—allows Burek to see how the helmets are working and the types of accidents that lead to injury—in theory. While the data keeps coming in, the company hasn’t yet found the right individuals to analyze the information and draw useful conclusions about which equestrian activities are the most dangerous or how helmet design can improve to better protect riders.
Burek, who’s also involved with the ASTM International (the organization formerly known as the American Society for Testing and Materials that develops testing standards for helmets), invited representatives from the U.S. Equestrian Federation to the last meeting, hoping they will also analyze and share data they’ve collected from shows.
Other sports have some research that looks at what types of impacts correspond to concussions. Turner is particularly interested in work being done by the neurosurgeon for the Australian Rules Football League.
ADVERTISEMENT
“They’ve created an assessment of individual blows based on watching film of the games,” he said. “They’re trying to validate that there are certain types of blows that are associated with concussions and others that aren’t. Since a fair number of concussions have no objective symptoms, some players may feel unwell but keep playing. Athletes aren’t great at reporting symptoms. So during the games they can have multiple spotters watching the film, and if they see a specific type of blow or reaction, they immediately pull the player. The doctor can make a determination just from watching the film, and it’s been validated really well. The NHL just started looking at that too.”
Keeping Heads Safe At Shows
Stewards complete accident/injury reports for any accident, whether a horse is involved, at USEF competitions. Fatalities and “serious injuries” are reported to the USEF immediately, and any accident with a suspected concussion must be reported by 6 p.m. the day following the accident.
“We collect a lot of data,” said Malcolm Hook, head of the USEF Safety Committee. “The difficulty is, are we collecting the correct data, and are we combining it well? [Chambless] is very aware of what we’re doing, and she hasn’t said we’re looking at the wrong things. Every accident/injury report form describes the circumstances involved with the injury.”
Eventing has taken the lead in collecting data around accidents, but Hook says hunter/jumper shows are catching up quickly. The two-page accident/injury report is thorough, asking about the footing, weather condition, type of jump, safety equipment (if any) involved, type of fall and details of the actual event. Stewards report the medical treatment the rider received, interview witnesses, and sometimes track down photos or videos of the fall. Hook said riders are often the best at describing the accident (if they’re conscious), but HIPPA laws mean that first responders may not give any medical information to a USEF official—even though the accident/injury reports are confidential.
“We have seen an increase in concussions, but I think some of that is the result of better reporting as much as anything else,” said Hook. “In 2016 and I hope 2017 we’re not seeing any unusual increases. In 2016 we had 219 concussions reported, and for the first three-quarters of 2017 we’re at 186, which is about the same as where we were last year.”
Hook rattled off other statistics: Sixty-five percent of head injuries at horse show occurred in conjunction with a jumping effort and 89 percent were injured while preparing for a class or competing. He pointed out that in raw numbers, the hunter/jumper world has five times as many concussions as eventing (yes, you read that right), but when accounting for number of overall starters eventing has more head injuries per competitor. Hunter/jumper, eventing and dressage rank first, second and third respectively in the raw number of concussions of all the USEF breeds and disciplines.
There’s also the question of return to play. Starting in 2018, GR849, a new return to play rule, kicks in for all sports. This rule addresses and expands on how concussions are to be handled, including the provision that stewards’ reports include the number of suspected concussions sustained at shows. Eventing has its own, stronger rule that implements mandatory suspensions after concussions, which riders can avoid by passing an ImPACT test.
Then there are helmets, the first line of defense against head injury. They’re important, but they can’t do everything.
“Helmets are designed to prevent severe TBI,” said Chambless. “Tests are based on protecting the brain against skull fractures and severe injury. They are not designed to prevent concussion. Concussion is acceleration/ deceleration.
“It’s a huge problem,” she continued. “So the technical breakthrough needs to happen at the acceleration and deceleration level to dramatically reduce concussions. People are looking at that. They’re trying to determine the threshold for the average human of acceleration of the brain against the skull before there’s a concussion.” 
There’s also a rule change proposal put forth by the USHJA that would require, among other things, concussion training for all professionals. USHJA President Mary Babick said that while there’s lots of support for mandatory concussion training from the USHJA board of directors, the rule still needs some tweaks. For example, should the rule apply to just the USHJA, or to all breeds and disciplines in the USEF?
“[USEF President] Murray Kessler has appointed me the head of a task force, which we’re assembling to see if we can get the rule amended so that all the affiliates are on board,” she said. “As an industry we are far behind the curve on this, and the USHJA is willing to be the trailblazer if the other affiliates aren’t ready.”
Concussion Resources
- Check out the USEF Learning Center video by Dr. Lola Chambless, titled “Concussions: Signs, Symptoms, and Helmet Safety,” usef.org/ learning-center/videos/concussions- signs-symptoms-helmet-safety
- The USEF has put together a wide variety of resources for equestrians about concussions and brain injuries: usef.org/compete/resources-forms/ rules-regulations/concussion
- You can watch a USEF Town Hall Meeting led by Chambless here: usef.org/network/ coverage/2017AnnualMeeting/0_ zoowhch7
- The Centers For Disease Control And Prevention’s Heads Up program has up-to-date information and resources for parents, coaches and providers about concussions and brain injuries, including free online concussion training and free, customizable hand- outs and posters: cdc.gov/headsup/ index.html
- To read the study in the Journal of Neurosurgery that determined that 45 percent of patients admitted to a hospital with a sports- related traumatic brain injury are equestrians, visit thejns.org/doi/ abs/10.3171/2016.1.FOCUS15613
Check out the author’s blog entry about writing this series.
This article appeared in the Feb. 26 & March 5 issue of The Chronicle of the Horse. The second part of the series, “Protecting Our Heads, Now And Down The Road,” appeared in the March 12 & 19 issue.
You can subscribe and get online access to a digital version and then enjoy a year of The Chronicle of the Horse and our lifestyle publication, Untacked. Or you can purchase a single issue or subscribe on a mobile device through our app The Chronicle of the Horse LLC.
If you’re just following COTH online, you’re missing so much great unique content. Each print issue of the Chronicle is full of in-depth competition news, fascinating features, probing looks at issues within the sports of hunter/jumper, eventing and dressage, and stunning photography.
What are you missing if you don’t subscribe?















