If you’d asked amateur rider and second-year medical resident Dr. Karley Koch to predict what would be the hardest part of working in Oklahoma’s biggest hospital during a global pandemic, she might’ve said she was worried about patients outnumbering the hospital beds or running out of personal protective equipment and risking her own safety.
But at the end of May, almost a month after the state has begun the process of reopening, she’s finding the worst part is how alone this disease leaves people, cut off from their support networks during their darkest hours.

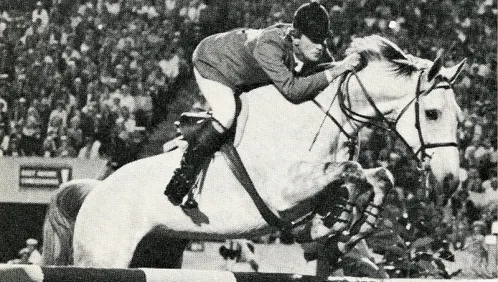
Dr. Karley Koch shows Silvia in the jumpers, and she’s just started being able to ride again now that COVID-19 related restrictions have eased up in Oklahoma. Jerry Mohme Photography Photo
As of May 1, Koch began a hospital services rotation, where she does inpatient medicine at the Oklahoma Health Center as part of her education at the University of Oklahoma Health Sciences Center in Oklahoma City.
That means she’s admitting people who are coming from the emergency room and will require a longer stay in the hospital, or people come in as direct admissions from the health care clinic.
During the time when the state was mostly locked down due to COVID-19—mid-March through the end of April—the hospital census was at an all-time low. Koch estimated it was at about 50% capacity, as opposed to during normal times when the ER is completely full, and doctors sometimes see people in beds in the halls.
The only patients in the hospital were the sickest of the sick. “When things started reopening, and people started going back to their doctors, we got this influx of really, really sick people who shouldn’t have gone without health care or seeing their doctors for a couple of months,” said Koch. “We’re seeing a negative side effect of the shutdown when people were scared of going anywhere at all, even necessary doctor’s appointments with their primary care doctor.”
Admitting people to the hospital is always emotionally difficult, said Koch, but the situation is particularly tough now, after the state’s reopening.
“I had a guy come in who, for these two months on pretty much lockdown, was showing signs and symptoms of pancreatic cancer,” she said. “He came in really sick and didn’t realize how serious things were.”
In order to minimize COVID spread, the hospital still isn’t allowing visitors, which means people don’t have the support of their families by their side during these devastating diagnoses.
“The patient I talked about earlier, having that conversation with him with his wife on speakerphone, it’s not the same. It’s really hard,” said Koch. “Having really difficult conversations with people about their end of life and what’s that like and making really hard decisions about end of life without having the support of their family there—it sucks. It’s hard on the patients, of course, but it’s really hard on us too. Having the family support there is just as good for the patient’s health as anything else.”
ADVERTISEMENT
Other unpredicted results from the pandemic lockdown? “When things started reopening, we’ve been seeing a lot of people having a little too much fun and ending up in the hospital,” said Koch. “Our list is either really, really sick people, which is really sad and awful, or it’s drug and alcohol detoxes. It’s been really weird.”
Koch’s also had to do her job without some of the support staff she normally utilizes. “People are under the impression that healthcare is untouchable from the economic downside of this whole shutdown, but that’s certainly not true,” she said. “Our clinic saw its lowest numbers ever, even though we were switching to telemedicine. People were canceling a lot of their appointments.”
This led to furloughs and downsizing. “It’s been really horrible,” said Koch, 27. “The only blessing to being a resident at this period in time—we don’t get paid very much anyway, we get paid hardly anything for how much work we do, but we’re getting paid totally separately from OU itself—so as a resident we haven’t really been affected by this. But my attendings, my nurses, the staff, the case managers, everyone that makes this thing tick has really taken a hit.”
She hasn’t run out of personal protective equipment yet, but that’s thanks to very conservative use. “I was on labor and delivery for the whole month of April, and I still have the same N95 mask that I got on April 1 that I did all of my deliveries in, and I still use it for COVID pending and COVID positive,” Koch said. “I’m allowed to change it whenever I really need to, but because of the shortages, I’ve been hanging onto my N95.”
She can swap her surgical mask once a day, but sometimes she uses the same one for longer. “It’s such a hassle trying to find one, that I’ve usually been wearing the same surgical for a week at a time,” Koch said. “It’s not ideal. That’s not being forced on us. We’re allowed to change them, but sometimes it’s more of a headache to try to get ahold of stuff like that than it is to just keep wearing it.”

Dr. Karley Koch has had to be conservative with her personal protective equipment during the COVID-19 outbreak. Photo Courtesy Of Karley Koch
And their COVID cases? What’s happened since Oklahoma started reopening? “We’ve all been holding our breath waiting,” said Koch. “Things reopened May 1, and we braced ourselves in the hospital.”
Three weeks after restrictions started to ease, the hospital began seeing a slight uptick in COVID admissions. “It’s not substantial yet. I’m not saying we’re overwhelmed by any means, but we had a down trend for so long, and today was the first day where we were going back up,” said Koch.
But there have been upsides to reopening too. For six weeks Koch wasn’t able to ride her jumper, Silvia, but her barn is once again allowing boarders to come.
“We’ve transitioned from one person out at a time, not in the barn at all, being handed the horse tacked, to now we have two separate tacking areas, and there can be two to three people at the barn at a time, just in separate locations, kind of staggered,” said Koch.
ADVERTISEMENT
As someone who’s relied on her horse to provide strength and stress relief, the period without seeing and riding Sylvia was particularly tough. “There was a point in time where my trainer was allowing people to come out and do pasture visits, so we could drive in—we couldn’t go anywhere near the barn—we could go to the pastures; we couldn’t go in,” said Koch. “One day I just went out there and sat down, crying. I was like, ‘I miss you so much.’ Getting back into it was really good.”
She’s also experienced an unexpected silver lining to her new situation in the hospital without support staff or family by the patient’s side.
“As residents, the team that I’m on this month, it has pushed us to be at bedside more than we ever have just because it’s necessary,” Koch said. “When [patients are] alone all day, taking that extra time to check on them or spend the extra time on the rounds in the morning, it’s important. Even without family being around, we’ve had more people thank us for our care—not even COVID related, just the normal stuff—more than ever. That part’s been nice.”
Koch is adamant that, despite the hardships created by the shutdown, it’s been a crucial component of preventing the spread of the coronavirus.
“I don’t think it’s over. We’re not out of this yet,” she said. “It’s going to come back somehow. It never went away. So it’s managing those influxes and those spikes is really what we’re after.”
She worries that people believe the worst is over since the state is opening back up, and they’ve stopped being careful.
“Not near as many masks are being worn anymore and not near as much social distancing as last month,” she said. “That’s a little scary, being on the health care side of things. I do understand where people are coming from. Quarantine was really hard, and it’s affecting our economy negatively; it’s hard. But don’t forget that you don’t see what’s going on inside the hospitals, which is kind of the whole point—protecting those spaces to be able to take care of those people when and if things get really bad.
“When we’re admitting people, even just the COVID pendings, they’re scared,” she continued. “They don’t have anyone there right now. They don’t have family. It’s hard. Whenever you see that every day, it’s easier to feel good about wearing your mask when you go to the grocery store.
“Please keep wearing your masks, and please keep doing your part and social distancing and not gathering in large groups of people and using hand sanitizer and washing your hands and all of the things,” Koch concluded. “It sucks, but it’s still helpful.”
Want more from Koch? She was featured in our Amateur Showcase series and was a guest on our podcast and spoke about the struggles of dealing with the coronavirus.